Spinal osteochondrosis is a chronic disease in which degenerative changes occur in vertebrae and intervertebral discs located between them.Depending on the site of spinal cord damage, they distinguish: osteochondrosis of the cervical region, osteochondrosis of the thoracic region and osteochondrosis of the lumbar region.To diagnose osteochondrosis of the spine, it is necessary to perform radiographs, and in the case of its complications (for example, the intervertebral disc herniation) - the spine MRI.In the treatment of spinal osteochondrosis, along with medication methods, it is widely used, reflexology, massage, manual therapy, physiotherapy and physiotherapy exercises.
Etiology and pathogenesis
On one scale or another, the osteochondrosis of the spine develops throughout the elderly people and is one of the processes of body aging.Previously or later, atrophic changes occur in the intervertebral disc, however, injuries, diseases and various spine overloads contribute to the previous appearance of osteochondrosis.The most common osteochondrosis of the cervical region and lumbar spine osteochondrosis.
About 10 theories of osteochondrosis have developed: vascular, hormonal, mechanical, hereditary, infectious-allergic and others.But none of them give a complete explanation of the changes that take place on their backs, on the contrary they are complementary to each other.
It is believed that the main point in the appearance of osteochondrosis is the continuous overload of the vertebral motor segment consisting of two adjacent beads.Such an overload can occur as a result of a motor stereotype - behavior, an individual way of landing and walking.Disordishes poster, sitting in the wrong position, walking with an uneven spinal column cause an additional load on discs, ligaments and muscles of the spine.The process may worsen due to the characteristics of the spine structure and the insufficiency of its tissue trophism due to hereditary factors.Most often, the vices in the structure are found in the cervical region and lead to vascular disorders and early appearance of osteochondrosis of the cervical spine.
The appearance of lumbar region osteochondrosis is most often associated with its overload during tendencies and severity elevators.A healthy intervertebral disc can resist considerable loads due to the hydrophilicity of the pulposal core located in its center.The core contains a large amount of water, and liquids, as you know, are slightly compressed.The breakdown of a healthy intervertebral disc can occur with a compression of more than 500 kg, while the disk changed as a result of osteochondrosis is torn with a compression of 200 kg.A load of 200 kg is experiencing a lumbar of a person's backpack weighing 70 kg, when holding a 15 -kilograms load in the body slope position before 200. Such a large pressure is due to the low size of the pulp nucleus.With an increase in the inclination to 700, the load on the intervertebral discs will be 489 kg.Therefore, often the first clinical manifestations of lumbar back osteochondrosis occur during or after lifting weights, performing housework, weeds in the garden, etc.
Destruction of the connective tissue of the fibrous ring of the disc, ligaments and capsules of the facial joints causes the response of the immune system and the development of aseptic inflammation with the swelling of the facial joints and their surrounding tissue.Due to the displacement of vertebral bodies, the capsules of the facial joints are stretched, and the changed intervertebral disc is not so firmly fixed by the bodies of neighboring vertebrae.Spinal segment instability is formed.Due to instability, spinal nerve violation with the development of radicular syndrome is possible.With osteochondrosis of the cervical spine, this often occurs during the scalp, with osteochondrosis of the lumbar region - during body slope.It is possible to form a functional block of the vertebral motor segment.This is due to the reduction of vertebral muscle compensation.
The intervertebral disc hernia is formed when the disk is moved back, the rear ligament rupture occurs and the disk extension in the spinal canal.If at the same time the core of the disk is squeezed into the cerebrospinal canal, then such hernia is called explosion.The severity and duration of pain with such hernia is much greater than the most unexploded.Disk hernia can cause radical syndrome or compression of the spinal cord.
With osteochondrosis, bone tissue growth occurs with the formation of osteophytes - bone results in the bodies and processes of the vertebrae.Osteophytes can also cause compression of the spinal cord or cause the development of radicular syndrome.
Symptoms of osteochondrosis of the spine
The main symptom of osteochondrosis of the spine is the pain.The pain can be acute of high intensity, it intensifies with the smallest movement in the affected segment and therefore makes the patient take a forced position.So, with osteochondrosis of the cervical spine, the patient keeps his head in the least painful position and cannot turn it, with osteochondrosis of the thoracic region, the pain also increases with deep breathing, and with lumbar region osteochondrosis it is difficult to decrease, rise and walk.Such pain syndrome is characteristic of compression of the spine of the spinal nerve.
In approximately 80% of cases, there is a dull pain of constant nature and moderate intensity.In such cases, after examination, the doctor should distinguish the manifestations of osteochondrosis of the spine from myositis of the back muscles.Metmece pain in osteochondrosis is due to excessive muscle tension, keeping the segment of the affected vertebral motors, inflammatory changes or significant extension of the intervertebral disc.In patients with such pain, a forced position is missing, but the restriction of movements and physical activity is detected.Patients with osteochondrosis of the cervical spine avoid sharp curves and tilts with their heads, with lumbar region osteochondrosis - slowly decrease and rise, avoid body slope.
Complications of osteochondrosis of the spine
The complications of osteochondrosis are associated with the hernia of the intervertebral disc.These include compression of the spinal cord, which is characterized by numbness, weakness of certain muscle groups of the extremities (depending on the level of compression), leading to the appearance of paresis, muscle atrophy, a change in tendon reflexes, urination and defecation.Intervertebral hernia can cause compression of the artery that feeds the spinal cord with the formation of ischemic areas (spinal cord infarction) with the death of nerve cells.This is manifested by the emergence of a neurological deficit (damaged movements, sensitivity, trophic disorders) that correspond to the level and spread of ischemia.
Diagnosis of osteochondrosis of the spine
The diagnosis of spinal osteochondrosis is performed by a neurologist or vertebologist.In the initial phase, spine radiography is performed in 2 projections.If necessary, they can shoot a special spinal segment and shooting in additional predictions.For the diagnosis of intervertebral hernias, the condition of the spinal cord is used and detects complications of osteochondrosis, magnetic tomography and resonance (spinal cord).An important role is played by MRI in the differential diagnosis of osteochondrosis and other spinal diseases: tuberculosis spondylitis, osteomyelitis, tumors, ankylose spondel, rheumatism, infectious lesions.Sometimes in cases of complicated osteochondrosis of the cervical spine, the exception of syringomyelia is needed.In some cases, if MRI is impossible, myelography is indicated.
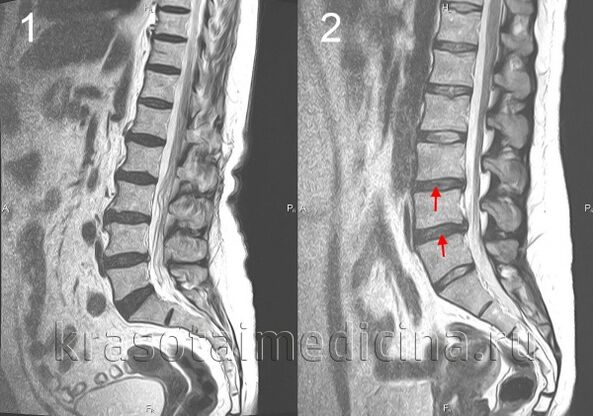
A target study of the intervertebral affected disk is possible using the discography.Electrophysiological studies are used to determine the extent and localization of nerve pathways, to monitor the process of their restoration during therapy.
The treatment of osteochondrosis of the spine
In the acute period, peace is indicated in the affected segment of the vertebral engine.To this end, with osteochondrosis of the cervical spine, the fixing is used using a chantz collar, with osteochondrosis of the lumbar region - bed rest.Fixing is also needed for osteochondrosis of the cervical region with volatility of vertebral segment.
In osteochondrosis drug therapy, non -steroidal anti -inflammatory drugs (NSAIDs) are used: Diclofenac, nimesulide, lornoxicam, meloxicam.With intense pain syndrome, analgesics are shown, for example, a central analgesic action of fluportin.To relieve muscle tension, muscle relaxants are used - tolperisone, thizanidine.In some cases, it is advisable to prescribe anticonvulsant drugs - carbamazepine, gabapentin;Antidepressants, among whom preference is given to the inhibitors of the opposite seizure of serotonin (Cersalin, Paroxetine).
In the case of a radical syndrome, hospital treatment is indicated.It is possible local introduction of glucocorticoids, anti -edema treatment, use of traction.In the treatment of osteochondrosis, physiotherapy, reflexology, massage, physiotherapy exercises are widely used.The use of manual therapy requires a clear respect for its application technique and special care in the treatment of cervical spine osteochondrosis.
Spine operations are mainly shown with a significant compression of the spinal cord.It consists of removing the intervertebral disc herniation and decompression of the spinal canal.It is possible to perform microdissecomy, disc reconstruction of the disk, replacement of the disk affected with an implant, stabilization of the spinal segment.

























